Release date: 2018-03-21
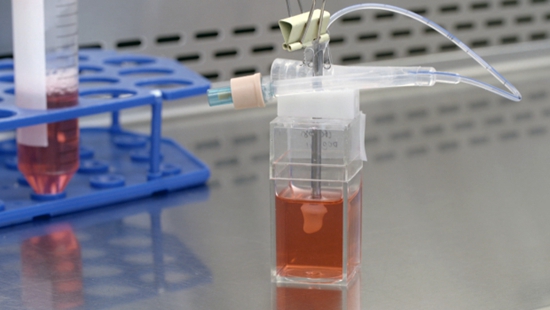
Mini heart soaked in the nutrient solution of the bioreactor
Along the needle, 17 different drugs enter 17 beating hearts. Human myocardial tissue is either calm or rapidly expanding and contracting due to strong stimuli, and the current flowing through the heart loses stability - which means that the heart owner died of a heart attack.
Dr. Kevin Costa, who led all of this, and his colleagues simply don't know what these drugs are and whether they will lead to terrible results. They just inject, observe, and record the results.
This is not a human life, there is no death in Costa's laboratory, only the rapid growth of current, data and cells. As the chief scientist of Novoheart, Costa led the team to develop an artificial mini heart. The raw material is human myocardial tissue. The finished product can beat like a real heart, only the size of the thumb.
They are far from being a substitute for the human heart, but they can play a major role in continuing the heartbeat of people. The team's immediate goal is to provide experimental subjects for drugs that treat heart disease.
According to a 2013 study by the Tufts Drug Research and Development Center, each new drug approved by the FDA (US Food and Drug Administration) was spent an average of $2.558 billion, and nearly half of the money was spent on failed products developed during the same period. Many drugs passed the layer test and eventually fell into the biological experiment stage.
"If you want to fail, you have to fail early," Costa said. If the results of the experiment accurately predict the adverse effects of the new drug, the Mini Heart will help those products that are destined to fail to receive a happy judgment and give way to more promising products.
A drop of blood "plants" a "heart"
Companies that provide drugs to the Costa team have published the identity of 17 drugs and compared them against real patient and mini heart test results.
The process of publishing the results is like a variety show, which is divided into three groups of “explain answers†​​through online video calls. The first group, all right. The second group, all right. The third group is wrong.
In the laboratory of Costa in Hong Kong, "Jelly" cans are displayed. The semi-solidified colloids in these bioreactors are culture fluids that provide nutrients and ensure acid-base balance. The canister is connected to the catheter and the culture fluid is transported through the catheter.
The mini heart beats in these jars like a hollow white peach. The Costa team sometimes calls them "canned hearts." Heartbeats come and go, each "Peach" has a special monitoring recorder, and the pulse curve fluctuates regularly on the screen.
"To create such a heart, we only need a drop of blood," said Novoheart CEO Lee Teng-wai.
Under the electron microscope, a drop of human blood is a square. Round, flat, lively, quiet cells roam in it. The PBM (peripheral blood mononuclear cells) that Li Dengwei is looking for is a blood system cell with a rounded nucleus. After "reprogramming", it can be transformed into iPS (inductive omnipotent stem cells), a seed of life.
iPS is the star of modern immunology. It is wide-ranging and can be transformed into a variety of human cells, which are derived into various tissues such as neurons, kidneys and retina. Japanese scientist Yamanaka Yamanaka won the 2012 Nobel Prize in Medicine for successfully inducing iPS using transcription factors.
In Costa's lab, biochemical inducers direct iPS to grow into a long, powerful cardiomyocyte, the most important material in the human heart.
At the same time, important tissue cells, such as "fibroblastic cells", have been cultivated. Costa ignored it in previous research and suffered a failure. Without these cell supports, the artificial heart does not form at all.
Next, Costa and colleagues mixed the cultured cells and hydrogels into a specially designed bioreactor. There is a mold in this glass jar, and the shape can be customized.
In the next few days, the cardiomyocytes clumped in groups and grew together, eventually producing fruit: a hollow chamber that can beat. It is much smaller than a fist-sized human heart, and its ability to beat is one-tenth that of normal human myocardium.
From undergraduate to postdoctoral, Costa has been engaged in biomedical engineering research, initially with the lungs. After his brother-in-law died of a heart attack, he turned to heart research. When he was an associate professor at Columbia University, he tried to "plant" a mouse heart in a petri dish with mouse stem cells.
In one experiment, he developed a small hole visible to the naked eye at the bottom of the heart. "It's over!" In frustration, he injected a little red stain into this obviously defective heart. After a few seconds, a red cloud fluttered rhythmically from the hole—the heart beats slightly, squeezing the dye out.
After repeated experiments, he finally got a rat heart that beats. In 2009, Lee Teng-wei found Costa: let's make a "heart".
Professor Lee Teng-wai of the University of Hong Kong has been an active advocate of stem cell technology. The Chinese biologist traveled to the United States and Australia when he was young. In 2007, iPS technology emerged in the scientific community, he began to look for partners, Costa is his alumnus of Hopkins University.
Scientists from the Mount Sinai School of Medicine in New York, the University of California, and the University of Karolinska in Sweden form an international team. When the image of myocardial contraction was magnified on the display screen in London, Chinese graduate students were slowly injecting the mixture into a pink gel in New York.

Mini heart
Beating big ambition
What Lee Tengwei wants is a mini heart that has the basic functions of a human heart.
In other words, the heart must be able to beat, but also to mimic the current conduction of the human heart, so that the myocardial fiber can shrink with the current.
At the same time, this team does not want to create a replica that is exactly the same size as a real human heart. Small, "convenient mass production, cultivation and testing."
The team designed the look of the heart: a three-dimensional chamber that "can beat and push the liquid." It is based on the human ventricle design, abandoning the natural combination of two ventricles and two atriums, is a "single room."
The Costa team believes that they created the world's first three-dimensional artificial heart. The myocardial tissue that was previously born in the laboratory is mostly two-dimensional, with only one layer of cells, and no structure.
Myocardial tissue has the ability to beat, and the power that gives it is electricity. The electrodes are placed in the nutrient solution of the bioreactor, mimicking the bioelectricity in the human body. The mini heart beats according to the frequency of the current. "Low frequency symbolizes calm state, high frequency jitter can mimic tension or motion state." Current dysfunction is a manifestation of cardiotoxicity.
The fluid injected into the heart changes the regular beat of the heart. If it is adrenaline, this heart will pounce, as if the human heart is manifested when the owner sees the lover or encounters danger.
A disturbance in cardiac current is observed to indicate the presence of cardiotoxicity. Drugs that cause heart discomfort often cause confusing currents.
What can be observed is not only the strength of stretching and contraction of myocardial tissue. The current, pressure, and volume are also recorded by the computer. "There are dozens of testable parameters for each organization." In the lab, a lot of data is being generated every minute.
Lee Teng-wei is very optimistic about the prospect of a canned heart. He believes that they "absolutely help to replace and reduce animal experiments." “An animal's heart is very different from humans, so animal testing often fails to reliably predict drug response. In contrast, human myocardial tissue can more effectively mimic the human heart.†These artificial hearts are not plagued by ethical controversies.
With the spread of medical personalization trends, the team hopes to use more individual blood to tailor the heart to test to understand the commonalities of diseases in a certain group of people and to select the best treatment for individual patients. Lee Teng-wei also believes that everyone in the future can have a "customized dedicated heart."
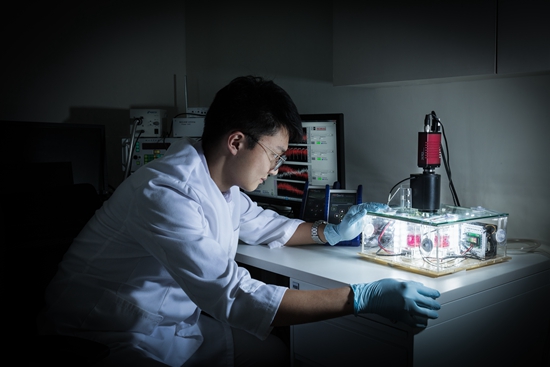
Novoheart laboratory staff is observing the mini heart
The market's response is slightly dull
In the BBC interview program, Lee Teng-wei was repeatedly questioned by the host: How far are we from the future you said? Can you give me a timetable?
This is one of the many mainstream media interviews Lee Teng-wai has accepted. The public has shown great interest in artificial hearts, imagining their potential to optimize or even replace animal experiments and human experiments.
The powerful opponent of these hearts is the "organ chip." This is a cell chip that is sized in submicron and can respond to a variety of stimuli. Like the canned heart, it is also cultivated based on stem cells. In January of this year, the Weiss Bioengineering Research Foundation of Harvard University published a paper introducing a chip constructed of myocardial tissue.
The market's response was slightly dull. In September 2016, Novoheart was listed on the Growth Enterprise Market in Toronto, Canada. This is a low-priced stock with a stock price of no more than 1.5 Canadian dollars. The stock price has dropped significantly over the past three years. The price per share this month has fluctuated around 0.5 Canadian dollars.
At the same time, the FDA has not disclosed the accuracy of the "synthesized simplified organ" test drug and its intention as an alternative measure for pathotoxicity testing.
Li Dengwei repeatedly stressed that the main purpose of Novoheart at this stage is to provide optimized screening options for new drugs before animal experiments, and does not want to replace them. There is still a lot to be done by this team. The next step is to further enrich and strengthen the function of this little heart to make it closer to reality.
“In the beginning, big pharmaceutical companies were very suspicious, repeatedly asking us about the physical connection between the mini heart and the real heart, and the accuracy of the prediction. Now they just want to know, where is your turning point?†“We give the medicine to you, How long will it give us results?"
The canned heart and its opponents belong to the future of a more distant, synthetic human organ. Organs grown in the laboratory will serve as a substitute for human experiments, stimulating the rapid development of new drugs. Alternatives to artificial heart may save the lives of heart patients like Costa Grandfather. According to data from the US Centers for Disease Control and Prevention in 2016, heart disease remains the number one enemy of global population health.
In the end, Lee Teng-wei took the humble smile of the Asians in the interview and cautiously said: "I can only say that in the not too long future."
Source: Zhongqing Online
High Resolution Distance Sensor
JRT produced the high resolution optical distance measurement sensor for 16 years with lower cost. Our distance measuring sensor have small size, high accuracy.
The laser range finder components is characterized by an above-average measured value output frequency, up to 8hz. The miniature laser distance module is also suitable for monitoring defined distance and height during transport.
Distance Measuring Sensor,Accurate Laser Measuring Sensor,High Accuracy Distance Sensor ,Optical Distance Sensors
Chengdu JRT Meter Technology Co., Ltd , https://www.irdistancesensor.com
